To understand and appreciate Adrenal fatigue, Chronic Fatigue Syndrome and Myalgic Encephalitis, one needs to understand and appreciate Cortisol.
To understand and appreciate Cortisol, one needs to understand and appreciate the adrenals.
Be warned !! – it will be a long journey to understanding, but there’s no other way.
So, let’s begin with the adrenals.
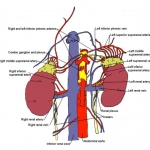
This pair of tiny (5×3×1 cm, 5 grams), complicated secretory glands sit one atop each kidney, in front of the 10th-11th rib on either side, where they are nicely protected from trauma, each supplied with blood by three arteries and each outputting its products into the big kidney vein, only an inch or two from the vena cava …….…..………………………………
Twin influencers, each sitting in its privileged position in the middle of town!
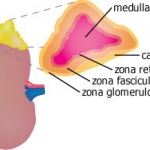
Each Adrenal has an outer, yellow ‘cortex” and an inner, dark red “medulla”.
The CORTEX, only 1 mm thick, consists of three layers, or “zones”, each of which makes a “Corticoid Hormone”:
The (outer) Zona glomerulosa makes mineralocorticoids, to control Sodium and Potassium in the urine (see Wikipedia).
The (middle) Zona fasciculata makes Cortisol, the “stress hormone”.
The (inner) Zona reticularis makes DHEA and Androgens.
The MEDULLA makes “Catecholamines”, the “fight or flight”, adrenaline-type hormones such as epinephrine and norepinephrine, which control skin, hair, muscle and gut responses to acute emergencies.
Each gland is enclosed in an active capsule, which does its maintenance and repair: this is unusual, because every other organ has a fibrous capsule which simply separates it from surrounding tissues (2).
THE HORMONES:
Cortisol (hydrocortisone), produced by the zona fasciculata,* is called a “glucocorticoid”, because it raises the blood sugar. It works by triggering conversion of glycogen (our glucose store) into glucose and when necessary, by converting proteins into glucose, in a process called gluconeogenesis, elsewhere (for example, in the muscles).
From
http://www.endocrinesurgeon.co.uk/index.php/adrenals-the-cortex-cortisol
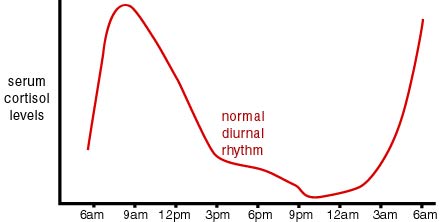
Released in the morning, with a maximum at 8AM and tapering through the day to an evening minimum, Cortisol aids in metabolism of fat, protein, and carbohydrates. In addition, it has a number of other functions: It is referred to as “THE STRESS HORMONE” because it is also released ** in response to Physical, Environmental or Emotional stress *** and reduced blood-glucose.
It decreases bone formation and chronically high levels can produce significant osteoporosis, especially in combination with Oestradiol deficiency, as in menopause.It reduces inflammation, but in doing so, suppresses the normal repair processes.
It reduces muscle proteins to amino acids, which the liver uses to make glucose; thus prolonged elevation of cortisol can lead to muscle wasting as well as thinning of bone.
Released in response to inflammation or injury, it counteracts the inflammation produced by “inflammatory cytokines”, but this benefit comes at the cost of immune system suppression, because in canceling the action of the cytokines it impairs the normal repair processes, including lowering white blood cell production and activity, which results in loss of the ability to fight infection and heal wounds.
In fact taking Cortisol can cause temporary diabetes, thereby allowing a mild infection to flare up into a severe problem.
* Cortisol is produced in other tissues, in lower quantities.
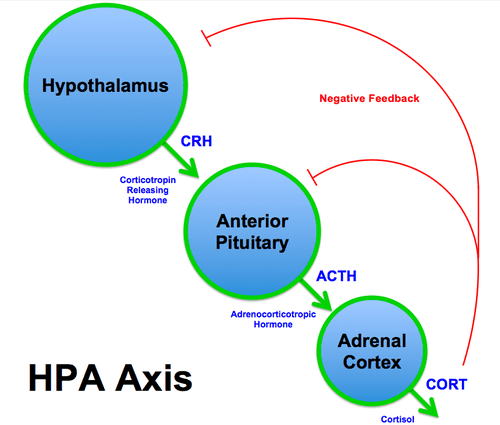
** The hypothalamus and pituitary, which together with the Adrenals constitute the HPA axis (the “HypothalamoPituitary-Adrenal axis”) *****, act together to control Cortisol production and release by the adrenals.
*** Emotional, physiological and physical stressors cause a release of Corticotrophin Releasing Hormone (CRH) in the Hypothalamus.
CRH travels in the portal passages of the Hypothalamus **** to the anterior pituitary (the “Adenohypophysis”), where it stimulates the production of ACTH (Adrenocorticotrophic Hormone). ACTH travels in the blood to the adrenal cortex, to stimulate production of cortisol.
**** Tiny tubes carrying hormones from the hypothalamus to the pituitary, to tell the pituitary what to do.
***** See the “NEUROSCIENTIFICALLY CHALLENGED” website, at https://www.neuroscientificallychallenged.com/blog/2014/5/31/what-is-the-hpa-axis
ADRENAL INSUFFICIENCY (Not “Adrenal Fatigue”)
Adrenal insufficiency can be divided into primary, secondary and tertiary.
Primary adrenal insufficiency (Addison’s disease) results from damage to or dysfunction of the adrenal gland itself. Production of all Adrenal hormones falls. Severe adrenal failure causes Addison’s disease.
Secondary adrenal insufficiency results from low production of AdrenoCorticoTropin (ACTH), by the pituitary gland. If your pituitary doesn’t make enough ACTH, your adrenal glands don’t make enough cortisol.
Tertiary adrenal insufficiency results from inadequate CRH release from the Hypothalamus, with resultant decrease in ACTH release. Causes include brain tumors, strokes and sudden stoppage of long-term steroid use, which is the usual cause.
PRIMARY ADRENAL INSUFFICIENCY: Primary insufficiency is clinically distinct from secondary and tertiary insufficiency. In primary insufficiency there is a decrease in both mineralocorticoids (aldosterone) and glucocorticoids (cortisol), whereas in secondary and tertiary insufficiency the aldosterone levels are virtually normal (the zona glomerulosa is independent of ACTH).
The most common signs and symptoms are: Weakness Nausea Abdominal pain Weight loss Dehydration Hypotension Lethargy Hyperpigmentation.
SECONDARY ADRENAL INSUFFICIENCY is much commoner than the primary form. The clinical features usually have a slow onset with many non-specific symptoms.
WHAT CAUSES PRIMARY ADRENAL INSUFFICIENCY (ADDISON’S DISEASE)?
- Surgical removal of both adrenal glands
- Autoimmune Diseases (when the body’s own immune system attacks itself)
- Granulomatous Diseases (e.g. tuberculosis and histoplasmosis)
- Metastatic malignancies (spread of cancers e.g. lung or breast cancer to the adrenal gland)
- Pharmacological steroid therapy
- Haemorrhage (bleeding in the adrenal gland, often as a result of anticoagulant therapy)
- Meningococcal septicaemia (Waterhouse-Friderichsen syndrome)
- Septicaemia (infection in the bloodstream) followed by loss of adrenal blood flow (5)
- Rare hereditary diseases
- Pneumocystis infection (as a complication of AIDS) Note that all of these conditions are of slow onset, except surgery.
TREATING PRIMARY ADRENAL INSUFFICIENCY
The aim of therapy is to replace the glucocorticoids and in some cases, mineralocorticoids, on an ongoing basis. Extra glucocorticoid is given for any illness or major stress (e.g. surgery, accident or infection). The patient can lead a normal active life, but must take precautions against emergenciesbyfaithful compliance with prescriptions, wearing a medical alert bracelet and staying in contact with support systems.
SECONDARY AND TERTIARY INSUFFICIENCY occur with hypothalamic or pituitary lesions, from Trauma, Surgery, Radiation, Infection, Tumours, Suppression of the adrenals after long-term steroid use. (6)
The clinical features of secondary adrenal insufficiency are similar to those above except that hyperpigmentation is not present (because ACTH is not elevated) and dehydration does not occur.
ADRENAL CRISIS
Adrenal Crisis is a life-threatening emergency and requires immediate treatment, with intravenous saline to correct the low blood pressure and Hydrocortisone to replace the cortisol.
In addition corrective treatment is given, for the cause of the Adrenal failure and any other problems. Adrenal Crisis usually presents as sudden hypotensive shock in two major groups of patients:
1. Previously undiagnosed patients subjected to major stress,
2. Previously diagnosed patients who fail to increase glucocorticoid replacement during a major illness.
CAVEAT: The prevalence of Autoimmune adrenalitis is only one in 20,000 persons and the symptoms preceding crisis are subtle: hyperpigmentation, fatigue, anorexia, orthostasis, nausea, muscle pain, joint pain and salt craving. Although surveillance and “a high index of suspicion” would lead to early diagnosis, this “prodrome” is often missed, but if the following protocol were applied to all patients presenting with fatigue, adrenal crisis would be truly rare:
DIAGNOSING ADRENAL INSUFFICIENCY (4)
Anyone presenting with fatigue gets a test for Cortisol done at 8AM.
If the Cortisol is lower than normal and especially if Sodium is low and Potassium high, an “ACTH stimulation” test is done to show whether the Adrenals can produce Cortisol.
This test will show whether the Adrenal function is normal or low and differentiate between primary and secondary failure is present, allowing early diagnosis and proactive, preventative therapy.
REFERENCES
(1) THE ENDOCRINE SURGEON, http://www.endocrinesurgeon.co.uk/index.php/adrenals-the-cortex-cortisol
(2) THE ADRENAL CAPSULE IS A SIGNALING CENTER CONTROLLING CELL RENEWAL AND ZONATION THROUGH RSPO3 Genes Dev. 2016 Jun 15; 30(12): 1389–1394. doi: 10.1101/gad.277756.116, PMCID: PMC4926862, PMID: 27313319 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4926862/
(3) Long-Term DHEA Replacement in Primary Adrenal Insufficiency: A Randomized, Controlled Trial: Eleanor Gurnell, Penelope Hunt, Suzanne Curran, Catherine Conway, Eleanor Pullenayegum, Felicia Huppert, Juliet Compston, Joseph Herbert, and V. Krishna K. Chatterjee J Clin Endocrinol Metab. 2008 Feb; 93(2): 400–409. Published online 2007 11 13. doi:10.1210/jc.2007-1134PMCID: PMC2729149, PMID: 18000094
(4) ADDISON DISEASE: EARLY DETECTION AND TREATMENT PRINCIPLES: A. MICHELS, MD, N. MICHELS, PhD, Am Fam Phys, 14/4/1 ;89 (7):563-568. see https://www.aafp.org/afp/2014/0401/p563.html and https://familydoctor.org/familydoctor/en/diseases-conditions/addisons-disease.html.
(5) ADRENAL INSUFFICIENCY IN SEPSIS, Djillali Annane 1 , . 2008;14(19):1882-6. doi: 10.2174/138161208784980626. PMID: 18691099 DOI: 10.2174/138161208784980626
(6) GLUCOCORTICOID THERAPY AND ADRENAL SUPPRESSION, Nicolas C Nicolaides, MD, PhD, Aikaterini N Pavlaki, MD, Maria Alexandra Maria Alexandra, MD, PhD, and George P Chrousos, MD, PhD, MACP, MACE, FRCP. Update: October 19, 2018, Bookshelf ID: NBK279156PMID: 25905379 https://www.ncbi.nlm.nih.gov/books/NBK279156/