SHOULD OUR THYROID HORMONAL ASSESSMENT BE REVIEWED?
Currently, our “system” says that to figure out whether a person’s thyroid balance is satisfactory in terms of keeping our cells working at maximum efficiency, all we need to check is the Thyroid Stimulating Hormone. However TSH is a signal sent by the Pituitary gland, to tell the Thyroid how much T4 to make.
THIS HAS NOTHING TO DO WITH THE REST OF THE BODY: the pituitary is merely ordering Thyroxine, to satisfy itself.
WHAT OUR MEDICAL SYSTEM IGNORES
Since FT3 is rarely, and rT3 never, measured, Physicians are unaware of the state of thyroid hormonal balance in the cells and organs: the body has no way of expressing its state of satisfaction, and other than T4/FT3 /rT3 we don’t have a dedicated test for thyroid balance.We can, however resolve the dilemma with minimum civil disobedience: let’s see FT3 and rT3 results and figure it out!
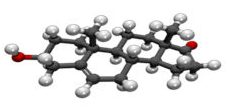
METABOLISM OF THYROXINE, THE “T4” HORMONE
T4 is converted preferentially to T3 rather than rT3 under normal circumstances, but when Cortisol output rises due to fasting or any other stress [1,2], FT3 production falls and rT3 increases, while TSH and FT4 are only minimally affected.
If rT3 goes up when T3 goes down, we can estimate the “strength” of the shift by dividing the T3 value by that of rT3; the ratio thus derived is a measure of the severity of the process and the depth of pathological deviation from normal T3/rT3 balance.
It has been observed that when the FT3/rT3 ratio is less than 20.0, hypothyroid symptoms appear; we differentiate this from true Hypothyroidism with a new term: “Functional Hypothyroidism”.
Clinical observation confirms that Hypothyroid symptoms coincide with this logic and that therapy with slow-release Triiodothyronine reliably relieves those symptoms.
TREATING FUNCTIONAL HYPOTHYROIDISM
If the patient takes T3 (slow-release,”SR” Triiodothyronine *), serum FT3 rises, rT3 falls and the ratio goes up.
Usually, FT3/rT3 exceeds 20.0 when the serum FT3 rises above 4.5, but a FT3 of 5.0-6.0 is the target of choice.
Treatment with SR T3 is safe and side effects (SE) are minimal.
The mildest SE is a feeling of being “high”, with enhanced vision and other sensory abilities, but some subjects have noted a hyper-reactive state, irritability, “antsiness” or increased pulse rate.
Therapy begins with 5mcg daily, increasing weekly by 5mcg/day, to a maximum 25mcg or until SEs occur: if SEs are noted, the dose is reduced to the previous level. TSH, FT4, FT3 and rT3 are repeated at a dose of 25mcg, or the dose which does not cause SEs and the dose is modified accordingly, to yeild a FT3 between 5.0 and 6.0.
Reverse T3 usually falls to less than 13 Nanograms/Decilitre when T3 exceeds 5.0 pM/Litre.
EFFECT OF THERAPY WITH TRIIODOTHYRONINE
The endpoint of therapy is elimination, or suppression, of hypothyroid symptoms, as judged by the patient.
Successful therapy reduces the perception of stress, whether or not the individual’s stressors are lessened and relapse is unlikely as long as treatment continues.
SRT3 can be discontinued if the stress is eliminated, but hypothyroidism will relapse if the stress recurs.
CAVEAT: weight loss may occur, but SRT3 MUST NOT BE PRSECRIBED FOR WEIGHT CONTROL !
ANCILLARY PRESCRIPTIONS
Iodine and Selenium supplements may help, but successful prescription of Triiodothyronine does not affect the patient’s requirement for other supportive hormone replacements or prescribed medications, excepting that drugs for Glucose and Cholesterol control, hypotensives, cognitive support, soporifics and psychoactive drugs can often be eliminated or minimised.
REGARDING THE “NORMAL” RANGE OF REVERSE T3
The normal level of Reverse T3, nominally 5 to 25, is difficult to assess. Similarly to T3 and TSH, it has been subject to error due to the inclusion of functionally hypothyroid subjects in the cadre of “normal” people whose thyroid profiles have been used to calculate the reference ranges.
Based on observation of approximately 300 cases and in line with their responses to therapy, my opinion is that especially since rT3 is a nonfunctional “waste” metabolite, the level is significant only because it gives laboratory evidence of excessive conversion of T4 to rT3. Ergo, estimation of “normal” for rT3 is unnesessary and perhaps obfuscatory.
Having said which, I would suggest a nominal “Normal” of 5-13 Ng/DL.
NOTES
Patients given Eltroxin or Synthroid during an episode of functional hypothyroidism, while T4 is being preferentially converted to rT3, experience marked worsening of their hypothyroid symptoms. This is because the T4 is converted to rT3, which has the effect of reducing T4 conversion to normal T3. Therefore their T3 level falls even further and the hypothyroid symptoms are exacerbated.
Patients who experience a stressful episode while on treatment for pre-existing true hypothyroidism, may suffer the same fate.
Dessicated Thyroid should not be used to treat stress-related functional hypothyroidism, because it is 70% T4 and 30% T3 and therefore may increase symptoms just as Eltroxin does.
Patients taking T3 (in a slow-release format) often reduce rT3 production to < 9 Ng/DL.
Since T3 usually penetrates the Pituitary and since the Pituitary actually uses its level of T3, not T4, to guage its TSH output, TSH often falls to <<1.0.
Reduced TSH output by the pituitary results in reduction of T4 production by the thyroid, so a T4 of 8 or less is often seen during SRT3 treatment. THIS IS NOT A CAUSE FOR CONCERN.
Most often, exogenous T3 enters the pituitary easily and TSH falls to a minimum. However in a small precentage of cases a high TSH is seen, in the face of high-normal T3 and very low rT3: this shows exclusion of exogenous T3 from the Pituitary and requires therapy with T4 …… This is the only scenario in which a prescription of T4, as Eltroxin or Synthroid, is appropriate.
NOTE: In 2014, two of my patients presented to an ER with FT3 of 1.7: both had cardiac failure of myxoedema.
TSH should be tested as an indicator of the Pituitary’s need for T4, but not for T3 balance.
The Normal for T3/rT3 being > 20, the optimal level should arguably, be 24-50.
The T3 range, currently skewed because a large, unrecognised percentage of our population is functionally hypothyroid, should be reviewed, reverted to the original 3.4 – 6.2 (or more) pMol/L
THIS TABLE WAS DEVISED FOR A PREVIOUS ITERATION: I INCLUDE IT HERE, “JUST FOR FUN”
| If T3 in Pm/L | T3,Ng/DL | rT3,Ng/DL | T3/rT3 | DIAGNOSIS | COMMENT |
| 2.8(newLo N) | 181.8 | 10 | 18.2 | Mild FH | Includes endemic hypothyroidism |
| 3.2 (old Lo N) | 207.8 | 11 | 18.9 | Mild FH | Need rT3 <11, to be Euthyroid |
| 5.0 (Optimal Lo N) | 324.7 | 25 (Lab High N) | 13.0 | Severe FH | Need rT3 < 16 to be Euthyroid |
| 5.0 | 324.7 | 20 (Lab High Mid) | 16.2 | Moderate FH | Need rT3 < 16 to be Euthyroid |
| 5.0 | 324.7 | 17 (Lab Low Mid) | 19.1 | Mild FH | Need rT3 < 16 to be Euthyroid |
| 5.8(New Hi N | 376.6 | 19 | 19.8 | Mild FH | Need RT3 <19 to be Euthyroid |
| 6.2 (Opt Hi N) | 402.6 | 21 (Lab Mid-High) | 19.2 | Borderline | Need rT3 < 20 to be Euthyroid |
| 6.2 (Opt Hi N) | 402.6 | 25 (Lab High N) | 16.1 | Moderate FH | Need rT3 < 20 to be Euthyroid |
| 7.6 | 493.5 | 25 | 19.7 | Still has FH | If rT3 = 25, Need T3 > 7.6 to be Euthyroid |
REGARDING TSH
In 2005 Leonard Wartofsky and Richard A Dickey wrote, (paraphrased, for brevity): “It has become clear that our reference ranges are no longer valid. We have more sensitive TSH tests and also, we now realise that previous reference populations included people with (low) thyroid dysfunction, whose high TSH levels led to a spuriously high reference range for TSH in the group. Recent laboratory guidelines from the National Academy of Clinical Biochemistry indicate that more than 95% of normal individuals have TSH levels below 2.5 mU/liter.”
In 2007 Martin I. Surks and Joseph G. Hollowell said as follows (paraphrased, for brevity)……
“The TSH median, 97.5 centile and prevalence of subclinical hypothyroidism (SCH) increase progressively with age. Age-adjusted reference ranges would include many people with TSH greater than 4.5 mIU/liter.” *
They continued: (”Without thyroid disease”), 10.6% of 20- to 29-yr-olds had TSH greater than 2.5 mIU/liter. *
In the 80+ year-old group “without thyroid disease”, 14.5% had TSH greater than 4.5 mIU/liter. *
TSH frequency distribution curves of the 80+ year-old group showed higher TSH.
The 97.5 centiles for the 20–29 and 80+ year-olds were 3.56 and 7.49 mIU/litre, respectively.
70% of older patients with TSH greater than 4.5 mIU/liter were within their age-specific range (up to 7.49)**. In spite of these findings (almost 100% of) our medical doctors preferred to think like Surks and Hollowell and the reference range for TSH has remained unchanged. ***
However to me, the implications are clear:
· Wartofsky and Dickey were correct and the upper limit of normal TSH should be 2.5, but they should have realised that 10.6% of their 20-29-year-olds were in fact, hypothyroid and should have excluded them. ****
· Surks and Hollowell would have done better to label the older folks hypothyroid, rather than concluding that “high TSH is normal for the older population”: what their findings mean is that a large percentage of the 80+-year-olds were hypothyroid and should have been excluded from calculations of normal.·
* AGE-SPECIFIC NORMAL, or “NATURAL NORMAL” makes no sense. “Normal” should be understood to mean the status of healthy humans aged 20-25 with no abnormal results for any test: any abnormal finding should disqualify the candidate for all estimates of “normal”.
These findings should not have been included in a calculation of “normal”.
** Any result >2.5 suggests hypothyroidism, so this implies that more than 14.5% of the
80+ year olds were hypothyroid: including them in the “normal” group means that 15+% of 80-yr-olds won’t get the treatment they need !
*** I dare suggest that one should apply fair logic to every scientific paper, so as to exclude glaring errors and prejudices like these from your belief systems.
**** Think about it – if I am right, since the thyroid hormone dictates the efficiency level of every cell and system in the body, and if 10.6% (or more) of the thyroid test study population should have been excluded from the calculation of “normal” thyroid hormone levels, then the parameters for all our other tests could be wrong and maybe a lot of tests might be invalid !
MESSAGE
· Many other hormones suffer the same fate as DHEA: Melatonin, Progesterone, Allopregnanolone, Testosterone and Thyroid hormone all go down over time, mostly by slow, gradual loss of production.
· In some people several hormone levels can “crash” suddenly, causing various symptoms of deficiency depending on which hormones are involved. This can happen with Melatonin in the “teens”, Progesterone and Allopregnanolone in the twenties, Testosterone in the thirties or earlier and particularly Oestrogen, which disappears in the early fifties but can fall to zero in the late thirties or early forties.
· Thus assesssment of “normal” in the presence of “natural age related hormonal change” is very difficult.
· To give medical investigators their due, a concerted effort is always made to include only the fittest individuls in the group evaluated. However there are instances in which unknown or ignored factors lead to a “curve ball” situation and consequent unreliability of an accepted “normal” range.
· IN SUMMARY, aberrations of hormonal production are pervasive and the interdependence of hormonal systems is delicate: test subjects should be BETWEEN AGE 20 AND 25 YEARS and ALL THEIR OTHER RESULTS SHOULD BE 100% NORMAL, for inclusion in studies to calculate a “normal” reference range for whatever test is to be evaluated.
REFERENCES
[1] Opposite effects of dexamethasone on serum concentrations of 3,3′,5′-triiodothyronine (reverse T3) and 3,3’5-triiodothyronine (T3),I J Chopra, D E Williams, J Orgiazzi, D H Solomon, J Clin Endocrinol Metab, 1975Nov;41(5):911-20, doi: 10.1210/jcem-41-5-911, PMID: 1242390. DOI: 10.1210/jcem-41-5-911,
[2] Diversion of peripheral thyroxine metabolism from activating to inactivating pathways during complete fasting, A G Vagenakis, A Burger, G I Portnary, M Rudolph, J R O’Brian, F Azizi, R A Arky, P Nicod, S H Ingbar, L E Braverman, PMID: 1150863, DOI: 10.1210/jcem-41-1-191 J Clin Endocrinol Metab, 1975 Jul;41(1):191-4. doi: 10.1210/jcem-41-1-191. https://pubmed.ncbi.nlm.nih.gov/1150863/
(3) The evidence for a narrower thyrotropin reference range is compelling
Leonard Wartofsky 1 , Richard A Dickey, J Clin Endocrinol Metab, 2005 Sep; 90(9):5483-8 PMID: 16148345 DOI: 10.1210/jc.2005-0455 .https://pubmed.ncbi.nlm.nih.gov/16148345/
(4) Age-Specific Distribution of Serum Thyrotropin and Antithyroid Antibodies in the U.S. Population: Implications for the Prevalence of Subclinical Hypothyroidism:
Martin I. Surks, Joseph G. Hollowell, The Journal of Clinical Endocrinology & Metabolism, Volume 92, Issue 12, 1 December 2007, 4575–4582, https://doi.org/10.1210/jc.2007-1499 01 Dec. 2007.
https://academic.oup.com/jcem/article/92/12/4575/2596923?login=true
(5) A new prognostic index in surgery and parenteral feeding: the ratio of triiodothyronine to reverse triiodothyronine in serum (T3/rT3 ratio) H.D. Calvey, W.J. Marshall, P.D. Marsden M. Davis
Front Endocrinol (Lausanne). 2018; 9: 97.Volume 5, ISSUE 3, P145-149, August 01, 1986:OI:https://doi.org/10.1016/0261-5614(86)90003-8 Published online 2018 Mar 20. doi: 10.3389/fendo.2018.00097 PMCID: PMC5869352 PMID: 29615976
(6) Higher Prevalence of “Low T3 Syndrome” in Patients With Chronic Fatigue Syndrome: A Case–Control Study
Begoña Ruiz-Núñez,1,2,* Rabab Tarasse,1 Emar F. Vogelaar,3 D. A. Janneke Dijck-Brouwer,1 and Frits A. J. Muskiet1 Front Endocrinol (Lausanne). 2018; 9: 97, Published online 2018 Mar 20. doi: 10.3389/fendo.2018.00097, PMCID: PMC5869352 PMID: 29615976 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5869352/
(7) Opposite effects of dexamethasone on serum concentrations of 3,3′,5′-triiodothyronine (reverse T3) and 3,3’5-triiodothyronine (T3) I J Chopra, D E Williams, J Orgiazzi, D H Solomon, PMID: 1242390, DOI: 10.1210/jcem-41-5-911
https://pubmed.ncbi.nlm.nih.gov/1242390/
(8) Effect of 3:5:3′-L-triiodothyronine in myxoedema, GROSS J, PITT-RIVERS R, TROTTER WR. Lancet. 1952 May 24;1(6717):1044–1045.
(9) A radioimmunoassay for measurement of 3,3′,5′-triiodothyronine (reverse T3). Chopra IJ. J Clin Invest. 1974 Sep;54(3):583–592. [PMC free article] [PubMed] [Google Scholar]
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC301591/
(10) Diversion of peripheral thyroxine metabolism from activating to inactivating pathways during complete fasting.Vagenakis AG, Burger A, Portnary GI, Rudolph M, O’Brian JR, Azizi F, Arky RA, Nicod P, Ingbar SH, Braverman LE. J Clin Endocrinol Metab. 1975 Jul;41(1):191–194. https://pubmed.ncbi.nlm.nih.gov/1150863/
(11) Concentrations of 3,3′,5′-triiodothyronine (reverse T3) and 3,3’5-triiodothyronine (T3) I J Chopra, D E Williams, J Orgiazzi, D H Solomon, PMID: 1242390, DOI: 10.1210/jcem-41-5-911 https://pubmed.ncbi.nlm.nih.gov/1242390/
(12) Diversion of peripheral thyroxine metabolism from activating to inactivating pathways during complete fasting, A G Vagenakis, A Burger, G I Portnary, M Rudolph, J R O’Brian, F Azizi, R A Arky, P Nicod, S H Ingbar, L E Braverman, PMID: 1150863, DOI: 10.1210/jcem-41-1-191 J Clin Endocrinol Metab, 1975 Jul;41(1):191-4. doi: 10.1210/jcem-41-1-191. https://pubmed.ncbi.nlm.nih.gov/1150863/
G. A. Harry, MB, BS (London), LMCC, FRCSC (urology), ABAARM (A4M, 2014).