A PARABLE ON HEALTHY AGING
ONCE UPON A TIME THERE WERE TWO CHIMPANZEES:
they were twins, but one was smart and the other, not so very.
On their third birthday each was given a toolbox, with a screwdriver, pliers, a hammer, a saw, a crowbar and a big knife.
The smart Chimp opened his toolbox and found that he could use the tools, lifting stones to find delicious worms, getting termites from their nests, opening walnuts, cutting coconuts, peeling oranges, squeezing things and generally making life easier for himself. He kept the toolbox in a dry spot inside his cave, took it with him everywhere and used the tools often, always cleaning and returning them to the box after use.
The unsmart brother loved his toolbox because it was the first birthday present that he could remember, but he never opened it and often left it out In the rain.
When they were about 26 years old, each somehow, on the same day, got caught in a trap set by a trapper who suffered from carpenteric dyslexia:
he made all his traps with autolocking doors, but he put the hinges on the inside.
The smart Chimp immediately noticed that his screwdriver would fit the screws which held the hinges and couldn’t keep his amusement down.
He sat for a while, giggling, then disconnected the door, put his ‘driver back into its box and walked out.
He tried to set his brother free, but couldn’t reach the hinges, the cage was made of steel, the crowbar wasn’t strong enough and the spaces between the bars were too narrow to let the screwdriver through, so he gave up trying.
He told the unsmart Chimp to open his toolbox but when he did, he found that the 26-year-old tools had rusted and stuck firmly together: he couldn’t even get them out of the toolbox.
The smart Chimp took his toolbox back to his cave and lived happily ever after, using his tools often and keeping them in good condition.
The unsmart Chimp was sold to a zoo, where he died at 33 from Alzheimer’s disease.
Q: WHAT’S THE POINT OF THIS IDIOTIC STORY ?
A: LOSS OF OUR HORMONAL “TOOLS”MAY BE NATURAL, BUT KEEPING THEM HAS BENEFITS
Due to hormone loss, we humans do not maintain perfect control over our functions permanently.
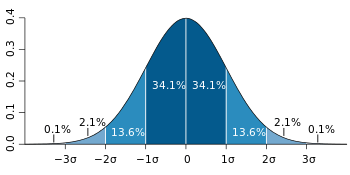
Kept healthy by our hormonal tools, we are fine up to age 25 or so, but thereafter we begin losing hormone production at a rate of about 1% per year, overall.
This produces a slowly accelerating decline in the efficiency of our metabolic management systems, which become “skewed” to a greater or lesser degree in one or another direction, depending on how our individual internal organs respond to reduced hormone levels.
In the opinion of Functional Medicine afficionados, our progressive loss of hormone production, though naturally occurring and 100% pervasive, is a disease and the resulting deviations from perfect health should be considered to be ill-effects of a pathological process.
From the Metabolic Medicine point of view, natural aging due to hormone loss is modifiable, if not truly treatable: hormonal balance is safely and easily acheived and with inexpensive, intuitive surveillance, can be perfectly timed.
Each individual, male of female, responds to hormonal loss with his or her own pattern of symptoms: depending on the individual organ’s sensitivity to lowered hormone availability there may be hair loss, weight gain, recurrent acne, dry skin, thin finger nails, allergies, high blood pressure, diabetes, autoimmune diseases, psychological change, cancer, neurological disease or other problems.
In addition stress, endemic to our modern lifestyle, can trigger suppression of thyroid function as an energy-saving reaction. When this happens all systems lose efficiency: muscles (including heart muscle) weaken and ache, the metabolic rate falls and we gain weight, loss of self-confidence leads to anxiety/depression and any pre-existing effects of hormonal reduction are accentuated.
While most people begin their disabilities at 26 (or earlier), many appear to be unaffected until much later. There is such a wide spectrum of “aging” effects that the majority are able to “carry on as usual” and the ones who fall by the wayside early in life are regarded as poor eaters, unhealthy due to bad habits or simply “unlucky”.
Nevertheless one thing is clear: no-one escapes the trap into which we are born and our “slide down the razorblade of life”, whether fast or slow, is inevitable.
As we age, most of the parameters by which our health professionals measure health remain stable and reasonably constant until some major system fails: tests for the function of the heart, blood vessels, kidneys, liver, lungs, intestines, endocrine glands, brain, bones etc remain sufficiently stable that hardly anyone shows obvious evidence of deterioration.
Unfortunately however errors are built into our surveillance plan:
[1] The hormonal balance, the measurable parameter which affects the function of all organs, changes steadily and can be monitored to give some indication of the general state of affairs, is ignored: decreasing test results are labeled “age-related” and considered “natural and normal for age”, thereby being relegated to the “interesting, but unimportant” file.
Let’s think about what we lose as aging progresses:
– Consider DHEA – it is precursor for Testosterone, Progesterone, Oestradiol, Cortisol and a host of microhormones which keep our parts working: all our cells, including thyroid cells, need it to maintain perfect function.
– Consider Testosterone: Zero “T” (normal 20-30 picomoles/Litre), often found in young women (I had a patient aged 23), is easily, safely treated with DHEA or “T” cream, but is usually ignored.
– Consider Progesterone: it rules the menstrual cycle, prevents PMDD, counteracts fatmaking Oestrogens and is raw material for Allopregnanolone (Q.V., Infra).
– Consider Allopregnanolone, darling of neuropsychiatry, which prevents and treats depression, ensures good sleep, is essential for memory, and maintains / repairs the brain. (12)
– Consider Oestradiol: it maintains the female “parts”, keeps the skin young and makes bones stronger.
…None of this is news, yet the progressive loss of all these hormones is accepted as “normal for age” and unremarkable: the ill-effects are accepted as inevitable and we are told to “live with it”!
[2] One hormonal system, the thyroid, is not tested accurately because TSH, which the pituitary gland sends out when it needs T4, is considered to be the only necessary thyroid test, although it only speaks for the pituitary’s need for T4 and has nothing to do with the body as a whole.
Consider the following:
– T3, your efficiency accelerator, is hardly ever measured and its “normal range” is unbelievably wide.
– Reverse T3, produced when the metabolic brake is applied and whole-body efficiency falls, is virtually never measured.
– Many anticancer drugs work by blocking T3, because cancer cells need it (all cells need T3).
[3] Mainstream doctors don’t test for vitamins and minerals, excepting Electrolytes, Vit B12, Iron, Calcium, Magnesium and Phosphorus. Although we know that an overload of Lead, Mercury and many other metals can be deleterious, tests for metal poisoning are almost never done and chelation treatment for metal overload is regarded as “quackery”.
WE CAN DETECT THE START OF HORMONE LOSS AND WE CAN REMEDY THE PROBLEM
A PLAN FOR HEALTHY AGING:
Age 5-15: Hormone information / awareness courses are taught in high school, to improve basic knowledge of the subject among the general population, facilitating the health practitioner’s surveillance and instruction of patients.
Age 15-25: A “wellness assessment questionnaire” and a short list of tests, most of which are inexpensive and easily available, are assessed by the family physician at age 15 and repeated every 5 years to age 25. thereafter or when as soon as symptoms of hormone loss begin.
Age 25-35: The wellness questionnaire and tests are repeated every 3 years.
The onset of symptoms, or an abnormal test result, triggers referral a brief explanation by the family doctor and referral to a health education professional (a well-paid paramedic, or nurse).
The the HEP reviews all aspects of hormonal balance, to ensure understanding of the diagnosis and proposed preventive therapy.
When the person concerned is ready to embark on (necessarily lifelong) hormone restoration and surveillance by testing, they themselves request a trial of therapy: this request is a mandatory prerequisite to prescription.
Refusal of advice or postponement of surveillance and/or therapy, is the individual’s prerogative, to be accepted without question by healthcare professionals, garnering no consequences.
FAQ
Q: WHAT’S THE POINT OF ALL THIS?
A: To reduce and delay body-system deterioration due to hormone deficiency. (1)
Q: WON’T IT BE EXPENSIVE?
A: It is a lot cheaper to prevent, than to cure. (2)
Q: HOW CAN WE AVOID OVERTREATMENT?
A: Repeated tests show the effect of therapy and the dose of hormone is adjusted accordingly.
Q: WHAT ABOUT HORMONE – DEPENDENT CANCER, LIKE HER-2 BREAST CANCER?
A: These cancers need the hormones to grow, but are not caused by the hormones.
A: Maintainance of DHEA, Melatonin, Progesterone etc deters cancer formation (4)
Q: PEOPLE WITH PCOS HAVE HIGH DHEA – WILL YOU CAUSE PCOS, BY INCREASING DHEA?
A: Not all have the high DHEA; it is caused by PCOS (not the other way around). (5)
Q: SUPPOSE TESTOSTERONE PRODUCES A PROSTATE CANCER?
A: That idea is wrong. Testosterone opposes Prostate Ca formation & low Testosterone aids it.
A: The Mayo Clinic still endorses the idea that P cancer should be treated by blocking T, (9), but
Testosterone prevents Prostate cancer and can be used as a treatment, in some cases. (6,7,8).
Q: DON’T HORMONES PREVENT PREGNANCY?
A: Only artificial hormones in birth control pills do, not hormones made by human glands. (10)
Q: AMD IS CAUSED BY THYROID HORMONE – CAN ThHormone MAKE YOU BLIND?
A: There is a link between higher levels of T4 and spontaneous AMD, not with Rx of T3 and T4. There must be some other factor that we have not as yet found: why would an essential hormone ruin vision? (11)
Q: WHAT ABOUT THYROID CANCER?
A: The story is the same as for other hormone-sensitive tumours: the cancer cells need thyroid hormone to grow, but TH does not cause the cancer.
REFERENCES
For brevity, only a few are listed. Many more are available through NCBI.
(1) The “multiple hormone deficiency” theory of aging: is human senescence caused mainly by multiple hormone deficiencies? T Hertoghe 1 Ann N Y Acad Sci 2005 Dec;1057:448-65. doi: 10.1196/annals.1322.035. https://pubmed.ncbi.nlm.nih.gov/16399912/
(2) The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary (Book).
https://www.ncbi.nlm.nih.gov/books/NBK53914/
(4) Hormone-sensitive cancer: Wikipedia, the free encyclopedia, https://en.wikipedia.org/wiki/Hormone-sensitive_cancer
(5) Adrenal Androgen Excess and Body Mass Index in Polycystic Ovary Syndrome
Carlos Moran, Monica Arriaga, Fabian Arechavaleta-Velasco, Segundo Moran
The Journal of Clinical Endocrinology & Metabolism, Volume 100, Issue 3, 1 March 2015, Pages 942–950, https://doi.org/10.1210/jc.2014-2569 https://academic.oup.com/jcem/article/100/3/942/2839480
(6) Does Testosterone Cause Prostate Cancer? Stephanie Watson — Healthline, September 18, 2018
(7) Testosterone as a Drug, Johns Hopkins 05/01/2018 Dr Denmeade https://www.hopkinsmedicine.org/news/articles/testosterone-as-a-drug
(8) Bipolar androgen therapy in men with metastatic castration-resistant prostate cancer after progression on enzalutamide: an open-label, phase 2, multicohort study Benjamin A Teply 1 , Hao Wang 2 , Brandon Luber 2 , Rana Sullivan 2 , Irina Rifkind 2 , Ashley Bruns 2 , Avery Spitz 2 , Morgan DeCarli 2 , Victoria Sinibaldi 2 , Caroline F Pratz 2 , Changxue Lu 3 , John L Silberstein 3 , Jun Luo 3 , Michael T Schweizer 4 , Charles G Drake 5 , Michael A Carducci 2 , Channing J Paller 2 , Emmanuel S Antonarakis 2 , Mario A Eisenberger 2 , Samuel R Denmeade 6 Clinical Trial, Lancet Oncol. 2018 Jan;19(1):76-86, doi: 10.1016/S1470-2045(17)30906-3. Epub 2017 Dec 14. https://pubmed.ncbi.nlm.nih.gov/29248236/
(9) Hormone therapy for prostate cancer is a treatment that stops the male hormone testosterone from being produced or reaching prostate cancer cells MAYO CLINIC, April 9, 2021 https://www.mayoclinic.org/tests-procedures/hormone-therapy-for-prostate-cancer/about/pac-20384737
(10) Birth Control Pills https://www.webmd.com/sex/birth-control/birth-control-pills
(11) Exploring the link between thyroid hormones and vision loss https://blogs.biomedcentral.com/on-medicine/2015/04/30/exploring-link-thyroid-hormones-vision-loss/
(12) Allopregnanolone, the Neuromodulator Turned Therapeutic Agent: Thank You, Next? Graziano Pinna*Department of Psychiatry, The Psychiatric Institute, University of Illinois at Chicago, Chicago, IL, United States. Front. Endocrinol., 14 May 2020 | https://doi.org/10.3389/fendo.2020.00236
https://www.frontiersin.org/articles/10.3389/fendo.2020.00236/full
Hormones RULE! - Tell your friends